The Western Trust Podiatry service provides specialist clinical services to those patients most at risk of foot health problems/conditions.
The Podiatry service provides specialist advice and treatment for high-risk patients suffering from complex nail and foot conditions. We hold outpatient clinics in GP practices and the main hospital sites.
Podiatry services are delivered by a skilled team of podiatrists and podiatry assistants. All our Podiatrists are registered with the Health and Care Professions Council and have completed a minimum of three years of accredited training at degree level or an equivalent qualification.
The service works closely with the Ulster University to support BSc (Hons) Podiatry students with work-based learning.
Referral to the Podiatry Service can be made via your GP or another health care professional or by contacting the Podiatry Team. Contact details are below.
All referrals are triaged on receipt as access criteria are in place for podiatry treatment.
Visit our Careers page for more information on careers in Podiatry
-
What We Do
The podiatry team work across a range of clinical settings in the hospital and community to provide a comprehensive foot health service, which includes:
- Nail surgery
- Podiatric management of foot pathology for patients with the following conditions: diabetes, vascular, oncology, rheumatology and renal disease
- Wound Care
- Musculoskeletal service – the treatment of mechanical foot problems with special appliances or insoles
- Integrated Clinical Assessment and Treatment Service (ICATS)
Podiatrists assess, diagnose and treat people with feet, ankle and lower limbs problems. They aim to improve mobility, independence and quality of life for their patients and to help reduce complications associated with all risk conditions affecting the feet.
These problems can be caused by a range of conditions, including:
- bone and joint disorders, for example, arthritis
- soft tissue and muscular pathologies
- neurological and circulatory diseases
- foot injuries and infections caused by sports and other activities
-
Diabetes Foot Care
 Diabetic foot disease is becoming an increasingly urgent health issue with more patients living with the disease are suffering from ulceration and amputation. The regional diabetic foot pathway launched in 2018. This pathway offers an improved service for people living with diabetes from Foot Screening, assessment, diagnosis of risk, education, protection and escalation through the Foot Protection Team (FPT), the Enhanced Foot Protection Team (EFPT) and the Multidisciplinary Foot Protection Team (MDFT).
Diabetic foot disease is becoming an increasingly urgent health issue with more patients living with the disease are suffering from ulceration and amputation. The regional diabetic foot pathway launched in 2018. This pathway offers an improved service for people living with diabetes from Foot Screening, assessment, diagnosis of risk, education, protection and escalation through the Foot Protection Team (FPT), the Enhanced Foot Protection Team (EFPT) and the Multidisciplinary Foot Protection Team (MDFT).Foot Screening – community based service for patients who live with or have recently been diagnosed with diabetes. A Podiatrist/Podiatry Assistant assesses patients and an individual care plan is agreed. Patients who are low risk will be screened every two years. Our service no longer offers a routine nail care service for those who are deemed to be low risk.
Foot Protection Team (FPT) – community based service offering assessment, treatments and education as per risk. Prevention and management of foot ulceration and they have direct access to the hospital based foot teams (EFPT)
Enhanced Foot Protection Team (EFPT) – hospital based service in Derry/ Londonderry, Omagh and Enniskillen. Patients can self-refer or are referred by any Health Care Professional with a deteriorating foot wound or red, hot swollen foot. They will get direct access to a team of professionals with the key skills necessary to assess, diagnose and initiate immediate treatment for diabetic foot disease. This team have direct access to the regional vascular and orthopaedic foot services in Belfast (MDFT)
 Multidisciplinary Foot Team (MDFT) – based in the Royal Victoria Hospital. This team comprises of Vascular and Orthopaedic Consultants, Interventional Radiologists, Podiatry and an Orthotist.
Multidisciplinary Foot Team (MDFT) – based in the Royal Victoria Hospital. This team comprises of Vascular and Orthopaedic Consultants, Interventional Radiologists, Podiatry and an Orthotist.This is a streamlined service available to all diabetic patients where early intervention and education can reduce the rate of ulceration and amputation. Patients are supported and encourage to manage their disease.
-
Help and advice for managing your verruca
What is a verruca?
Can be also known as plantar wart which is caused by the human papilloma virus (HPV) affecting the skin. Usually located on the sole of the foot but can occur on any area of the foot.
What do they look like?
They are commonly an area of thickened skin which has a cauliflower appearance with small black dots. They can vary in size of which you can have a single one, multiple or may spread to form a cluster. Usually painful if pinched and can be painful if located on a weight bearing surface.
What causes them?
A strain of the Human papilloma virus (HPV) which is contracted either through close skin to skin contact or indirectly from contaminated objects like towel, bath mat, socks or footwear and from floors of communal areas of swimming pool or gyms.The virus enters the skin through any small or invisible cut or abrasions and is more easily caught if skin is wet/moist or even dry/rough.
More commonly affect children but can affect adults.
They can be persistent and may take from 6 months to 2 years to clear.
How to prevent verrucae spreading?
- Wash your hands after touching it, try to prevent scratching or picking
- Change socks daily
- Do not share footwear, towels and avoid using same bath mat with any other house hold member
- Do not walk bare footed in public places, either cover the verrucae with a plaster or wear flip-flops when using communal area e.g. at swimming, gym etc.
- When self- treating and using a file to the verrucae, do not share the file with anyone else, use on any other area of foot and discard after episode of care is complete.
What to do if you have verrucae?
If painless then no treatment is required. The body’s own immune system recognises the virus and will fight the infection.
Evidence suggests many cases will disappear within 6 months although can take longer of up to 2 years.
Self–treatment
- File the area regularly with an emery board can help to stimulate the body’s own immune response and helps to maintain and prevent the thickened overlying skin.
- You can consult your local pharmacist who can advise on use of topical gels/ointments/paints and follow the instructions given carefully.
- No treatment is 100% effective and outcomes vary from person to person.
If self – treatment has failed and your verrucae are very painful you may require further advice and treatment from a qualified podiatrist.
Western Trust Podiatry do not offer verruca treatment.
-
Musculoskeletal Service (MSK)
 The Musculoskeletal Service treats patients with chronic and acute pain in the leg and foot, or patients with structural problems in their feet and legs that could lead to symptoms in the future. The Specialist Podiatrists will assess the way in which your legs and feet are working when you are walking and standing. This will lead to a clinical diagnosis and an individualised treatment plan which could include:
The Musculoskeletal Service treats patients with chronic and acute pain in the leg and foot, or patients with structural problems in their feet and legs that could lead to symptoms in the future. The Specialist Podiatrists will assess the way in which your legs and feet are working when you are walking and standing. This will lead to a clinical diagnosis and an individualised treatment plan which could include:- Insoles or Orthotics
- Strapping and splinting
- Stretching, Stability and Strengthening exercises
- Footwear advice

For Complex Biomechanical issues we have three specialised gait labs based in Gransha Park, Omagh Hospital and the South West Acute Hospital.
Patients can self refer or be referred by GPs, Physiotherapists and other health professionals who deem referral appropriate to the Biomechanics Service.
Patient compliance is a critical element of a successful outcome.
Achilles Tendinopathy
The Achilles tendon is the biggest and strongest tendon in the human body. Achilles tendinopathy is a condition that can cause pain, swelling, stiffness and weakness of the Achilles tendon. It is a very common injury reported in runners, however, it is not exclusive to this population as people who have a more sedentary lifestyle will also suffer from it.
Pain generally tends to be worse in the morning, or during and after exercise. Some swelling and/or pain can occur around the tendon and calf area – most often in the areas shown below.
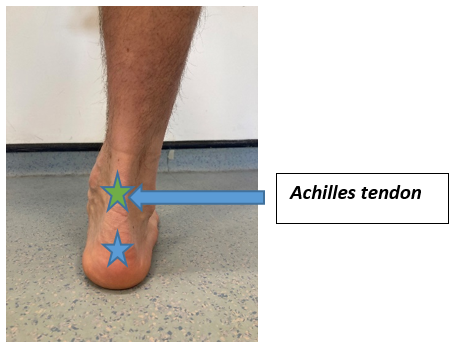
The blue coloured area is where the Achilles tendon inserts into the heel bone and the green coloured area is roughly the mid portion of the Achilles tendon. The tendon may be very tender to touch and you may have increased discomfort wearing shoes that press against it.
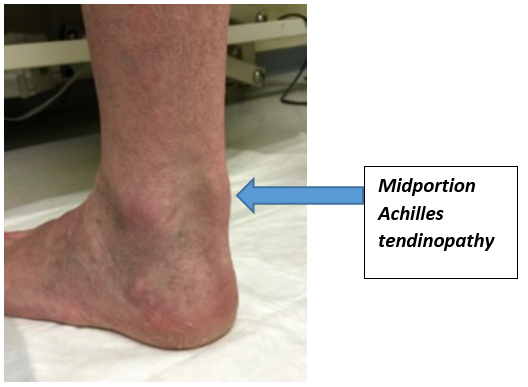
The pain can be in the midportion of the tendon (Midportion Achilles tendinopathy)
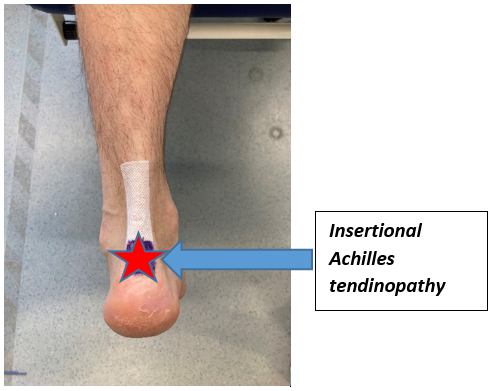
Or at the insertion of the Achilles tendon into the heel bone (Insertional Achilles tendinopathy).
The reasons for developing Achilles tendinopathy are varied but there are some common factors that seem to be important. The research consistently shows that reduced strength and endurance in the calf muscles is a major factor in developing Achilles tendinopathy. Also, being overweight will add more stress to the already struggling tendon. Footwear choice is important as the wrong shoes may nip the tendon and aggravate the problem.
Treatment of Achilles tendinopathy commonly involves loading based exercises. This basically means exercises for the affected muscle/tendon unit with the aim that it improves strength and endurance and reduces the symptoms.
Please don’t expect things to improve overnight though. It can take time for the tendon and muscles to adapt and improve. You may also find heel raises are useful to reduce the stress on the Achilles tendon while you are doing the rehabilitation, however, if they are uncomfortable, causing an increase in pain or other any other issues, then please remove them.
Bunions (Hallux Valgus)
What is hallux valgus?
Hallux valgus (also known as bunion) is a bony bump on the inside of the foot at the base of the big toe with the big toe tilting towards the second toe.
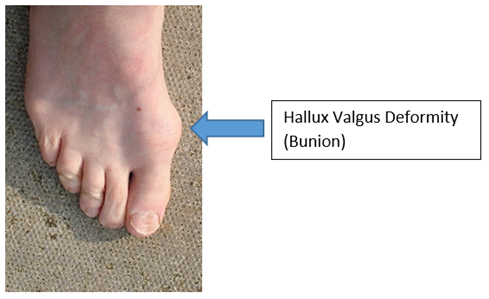
Many people who have bunions do not get any real problems with their feet and nothing needs to be done. Some people will however get pain around the big toe or problems with their shoes.
The bump can make foot wider and it can be difficult to find shoes which are comfortable
The bump can rub on shoes and become red and swollen and in some cases the skin can blister.
Some people with bunions go on to have problems with their smaller toes too.
What causes hallux valgus?
Inherited factors and the shape of the bones in feet can cause bunions. Footwear which does not fit well probably has a role in making bunions more uncomfortable and increasing problems in the future.
What tests may be done?
You do not need any x-rays or special tests to diagnose bunions, these are only used for planning surgery.
What can you do to help your bunion?
There are many non-surgical treatments that can help.
Footwear: One of the most important things you can do to help is to wear the right footwear. You should try to wear wide shoes with a low heel that fit you comfortably. Shoes with laces or an adjustable strap are best as they can be adjusted to the width of your foot.

Do not wear high heeled, pointed or tight shoes as this will make your pain worse.
Diet: Losing weight will reduce the strain on your feet.
Medication: Painkillers such as paracetamol can reduce the pain. Follow the advice from your community pharmacist or other healthcare professional about taking medication. It is important to take medication regularly.
Exercise: helps build the strength of the small muscles in your feet, which can take the strain off the toes and we think help to delay or stop problems getting worse.
What else can be done?
Most patients with bunions respond well to non-surgical treatments, especially changing their footwear. Where these have been tried and failed then there may be other options. If your pain does not start improving after a period of 3 months of following the advice above, please get referred to your local Podiatry Department to see a healthcare professional who can assess your foot.
Some patients may be referred on for Orthopaedic footwear or a surgical opinion.
Surgery
Surgery is considered in patients who have significant problems with their bunions and have tried non-surgical management which has not worked usually over at least 12 months.
An operation will not give you an entirely normal foot, but it will correct the shape of the big toe and narrow your foot back towards a more usual shape.
The aim of bunion surgery is to straighten the big toe and make it more comfortable. There are several procedures for bunion surgery and the best surgery for you depends on the size of your foot.
For most people the surgery is a bony surgery where the bones of your toe are cut and reset to straighten your big toe. This is called an osteotomy, some people who have developed arthritis in their big toe joint need a different type of operation where the big toe joint is surgically stiffened (fused). Very occasionally if your foot is more complicated an operation would be done further back in the middle of your foot to help straighten and support it.
Bunion surgery is largely very successful with around 85% of people happy with the outcome but as with any operation there are some risks.
After foot surgery, it may take 3-6 months for you to be back to your normal level of activity where you will be able to work standing all day, however every person is different.
Painful Big Toe Joint (Hallux Limitus or Rigidus)
The big toe joint (called the metatarsophalangeal joint or MPT joint) is an important joint that needs to be able to bend for the foot to work as efficiently as it should. Sometimes, for a variety of reasons, the joint can become stiff and make walking painful at this area – and sometimes it can become so bad that it results in a complete loss of movement.

Footwear is important in these cases. If the joint cannot bend, then a shoe with a stiff sole – or rocker sole – can be useful.

A shoe with a decent heel height may make symptoms worse as this will ask more of the joint and so may be best avoided – or at least limited.

Plantar Fasciitis
Plantar heel pain
There can be many causes of pain under the heel, but probably the most common one is irritation to the plantar fascia – sometimes called plantar fasciitis.
The plantar fascia is a band of thick tissue which runs from your heel bone to your toes. If you bend your big toe back, you should see it become prominent on the sole of your foot.
It helps to support the arch of your foot, but if it gets overloaded it can become thickened and cause discomfort under your heel and along your arch.
On the picture below you can see the bands of the plantar fascia, with the star indicating the most common site of pain.

A classic symptom of plantar fasciitis is pain on the first steps after getting up from a period of sitting or first thing in the morning when getting out of bed. It can be most painful under the medial plantar aspect of the heel pad – the area starred in the picture above. Sometimes this pain eases off a little when walking, only to come back again when you stop for a rest.
So what causes Plantar Heel Pain (Plantar Fasciitis)?
- Long periods of standing or walking or a sudden increase in activity levels (overuse).
- Being overweight will increase the load going through the foot, putting more pressure on the plantar fascia.
- Inappropriate footwear tightness/ weakness of the lower leg muscles
It is therefore important to maintain strength and flexibility in the muscles of the feet and legs to help manage and prevent the symptoms of plantar heel pain.
What can help?
- Adequate rest/ reduction of activities.
- Weight Management
- Appropriate footwear – this is important to help support the function of the plantar fascia. A trainer or a shoe with a cushioned sole can be very helpful.

- Stretching and strengthening exercises as shown below.

- A small heel raise or heel cushioning may help to reduce the pain whilst you are doing the rehabilitation. However, if they are uncomfortable or increase symptoms, then stop wearing them.
- If symptoms do not resolve, a Podiatrist may provide orthotics for additional foot support that may be beneficial.
-
Footwear
Wearing the correct footwear is very important to protect and support your feet.
What to look for:
- Shoes should be wide and deep at the toe box, to give your toes plenty of room.
- The heel of the shoe should be firm when squeezed.
- The toe box should bend as this is where our feet naturally bend when we walk
- Shoes should be supportive and have a velcro strap or lace, to secure your foot within the shoe reducing friction and blisters.
Trying on new shoes:
- When purchasing shoes you should always try them on and walk about the shop in them
- Feeling around the toe box ensuring you can’t feel your toes pressing/bulging
- Approximately 1cm gap from top of toe to the top of the shoe
- Foot should be held securely within the shoe once fastened
- They should be free from any prominent stitching on the inside which may cause rubbing.
- Shoes should not need to be ‘broken in’
Top tip
Tracing around your foot with a pen and paper and cutting it out gives you an idea of your foot shape & size. You can bring this template with you better visualise if the shoe will be a good fit for you.
What to avoid
Sandals, flip flops, high heels, narrow and slip on shoes should be avoided as these increase the risk of causing painful feet.
Insoles
If you have insoles for your shoes, look for shoes were the insole already in the shoe can easily be removed. Then place your insoles into the shoe.
If the inner shoe insole is not removable, place the insole in and try on ensuring it is not too tight a fit.
-
Home Visits
Western Trust Podiatry Service provide a home visiting service to patients who are totally chair or bed bound. On exceptions, a temporary home visit may be provided to patients who have experienced an acute episode of illness and clinically too ill to be expected to travel to a clinic.
The Podiatry Service encourages all patients to attend their local community clinics for a number of reasons which include being treated within a more appropriate clinical environment.
Please be assured, that by treating a patient at home, the podiatry care is no less than those who attend a clinic, it is simply that the service has limited care options when seeing a patient at home.
 Patients who are not eligible to receive a home visit include:
Patients who are not eligible to receive a home visit include:- Patients who attend other NHS appointments e.g. GP, hospital appointments.
- Patients who attend the hairdresser, shopping, post office, library.
- Patients who visit their family or friends.
- Patients who attend day centres.
The service is aware there may be situations when the patient’s circumstances are out with these criteria. In those situations, the clinician will discuss these changes with each person individually and mutually agree a decision regarding their eligibility.
-
Nail Surgery
In certain circumstances, despite conservative treatment, some toenails may require to be removed, either partially or totally.
Prior to any surgery a detailed assessment will be completed by the podiatrist to ensure that there are no contra indications to carrying out the procedure. Surgical and non-surgical options will be discussed with the patient and a treatment plan developed.
Surgery for full or partial nail removal is carried out under local anaesthetic which will be administered by the Podiatrist. The procedure normally takes about forty minutes. Comprehensive pre and post operative advice will be given by the podiatrist if surgery is required.
Normally full healing takes place in 6 –12 weeks. During this time the patient will be shown how to redress their toe and will be required to carry out redressing as required. Nails treated by our Podiatrists result in no re-growth of the nail in over 95% of cases.
Nail surgery is provided in several locations across the Trust area:
- Omagh Hospital and Primary Care Complex
- South West Acute Hospital
- Waterside Hospital
To prevent ingrown nails
- Do not cut your toenails too short
- Cut straight across the nail and file the edges
- Do not wear shoes that are too tight or do not fit properly
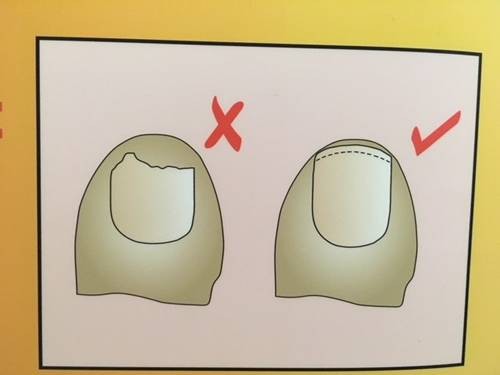
Cut toenails straight across the curve of the nail
A patient referred to Belfast Trust Podiatry Service for a problem nail condition will attend an initial appointment for a full podiatric assessment and diagnosis of the problem. This allows the patient to consider the options available and to ask questions to ensure an informed decision on treatment.

Nail surgery is the process of removing part or all of a nail under local anaesthetic. In most cases, the nail bed is treated with a caustic agent to prevent regrowth of the nail.
-
Children's Feet
Podopaediatrics is an area of Podiatry focusing on the diagnosis and treatment of childhood disorders of the foot and lower limb. We work in Woodview Assessment Clinic in Gransha Park.
Generally concerns regarding children’s feet and lower limbs such as flat feet, knock knees and in-toeing may not require anything other than advice and reassurance.
- Flat feet- it is natural for young children to have flat feet. As muscles begin to grow and strengthen an arch will appear. If your child has not developed an arch by the age of 9 or 10 a podiatry assessment may be advised.
- In-toeing- children who in-toe are usually otherwise healthy and although this may present some early challenges, your child can be expected to lead a normal and active life. If in-toeing persists to age 8 or 9 a podiatry assessment may be recommended.
- Knock knees- this is where the knees point inwards to face each other and usually improves after 4 years of age.
The treatment we provide can range from footwear advice and education to care for the young vulnerable foot as they grow and develop to ensure what footwear type’s parents should consider and frequency they get their child’s feet measured.
Orthotic treatment when appropriate can be issued used a range of precast devices to custom milled Cad Cam orthotic intervention with our own in house appliance centre based at Gransha allowing for orthotic adaption and manufacture at our gait lab Hub.
Stretching advice is also a key component in our education and advising on warm up/cool downs for sports to encourage good habits at an early age group into adulthood.
There may be occasions when biomechanical abnormalities require intervention. The podiatrist will provide an initial assessment, diagnosis and treatment which may include footwear evaluation and advice, foot health education and sometimes the provision of special insoles. The treatment plan may require onward referral to another service or appropriate consultant.
Strength and Proprioception
Now it is time to build some strong muscles at the front and back of the lower leg.
FAB FACT: These activities increase your proprioception with the added bonus of coordination. Your brain is working overtime with hand-eye coordination and ankle proprioception!
So many great things happen to children with these activities – proprioception, coordination, power development and self-confidence.

Toe Lifts
Stand up and lift your toes off the floor – as if you were trying to touch your knee with their toes. Do this at least 10 times, first with your toes straight, them with them curled in a little. Do this twice on each leg to help strengthen the muscle at the front and side of the lower leg.
Toe Lift Game

Sit down this time. Using small soft toys or sticky darts pick them up using your toes only.
Tiptoe Standing
Standing with feet slightly apart, go onto tip toes slowly and as high as possible. You can hold on lightly to something if you are a little wobbly. Count to 2 then come down again slowly. Do this 10 times if you can. You can place your hand above your child’s head as a target for them to reach. *Make it harder by doing it on one leg.
Single Leg Balancing

A simple yet very effective exercise. Stand up and take one foot off the floor. Try to balance for a count of 10 without moving the foot that’s on the floor. Repeat 2-3 times on both legs. *Make it harder by playing catch and throw with a ball at the same time or by standing on a wobbly cushion.

Jumping and Landing
Starting with a two-feet, jump from a stable surface and land on one-foot. Make sure to bend the knee on landing and try to “stick on landing” i.e. once you land, stop, find balance and don’t jump around. You can then jump from one-foot and land on the same foot. *Make it harder by adding a target to jump to – a spot on ground, a chalk mark etc.
Bridge pose

Great for strengthening your hips, tummy and leg muscles. Lie on your back and bend your knees up, keeping your feet flat on the floor, legs slightly apart. Push up so your bottom lifts off the floor and make a straight line down your tummy all the way to your knees. Hold this really still for a count of 10 them come down slowly. Repeat this several times. *Make it harder by pointing one leg away and balancing on the other one?
Bear walk
This exercise is super for strength all over. Start on the floor on your tummy. Lift yourself up onto hand and feet and move forwards, backwards, sideways, anyway you want. How far can you walk like a bear?
-
Renal Podiatry
 Individuals with Chronic Kidney Disease (CKD) have an increased risk for foot ulceration and lower limb loss.
Individuals with Chronic Kidney Disease (CKD) have an increased risk for foot ulceration and lower limb loss.Declining kidney function is an independent risk factor for foot ulceration and lower extremity amputation with a greater risk identified in individuals with Diabetes Mellitus (DM) and who require Haemodialysis (HD).
The Western Health and Social Care Trust Renal Podiatry service is located within Altnagelvin Area Hospital and Omagh Hospital and in particular is available to those with End Stage Renal Disease (ESRD) who receive Haemodialysis.
The Renal Podiatrist role focusses on early recognition of high-risk foot concerns with regular screening and follow up. This involves the evaluation of lower limb circulation and loss of sensation of the feet, the provision of treatment focused on relieving symptoms that enable and maintain independence, function and wellbeing, in conjunction with targeted education, and empowerment of the individual.
This service provision includes assessment and management of complications such as foot ulceration as part of a multidisciplinary team in order to help reduce foot disease related hospitalisations and amputations in individuals with chronic kidney disease.
The Renal Podiatrist also acts as a supportive resource to Podiatry colleagues and health care providers who are involved in the care of individuals with CKD.
-
Fungal Nail Infection
Fungal nail infections are very common and whilst can be unsightly, are not harmful.
The infection may cause nail to become discoloured (yellowish/brown) and sometimes it may become thick and crumbly.
These are commonly picked up from communal areas such as changing rooms and swimming pools.
It can also be spread by sharing towels, footwear and hosiery.
Hot sweaty feet and dry cracked feet are ideal breeding grounds for the infection.
You can reduce the risk of picking up a fungal infection by having good foot hygiene, always drying between your toes after bathing, keeping your skin in good condition with regular moisturising and avoiding walking barefoot in communal areas such as changing rooms and swimming pools.
Treatment is not always necessary.
These nails can be managed by regular filing to reduce thickness, to maintain comfort and improve appearance, however the Western Trust Podiatry is unable to facilitate this.
Treatment options
Fungal nail infections are very resistant to treatment; however below are best management options to consider.
- Antifungal lacquers can be obtained from pharmacy or GP prescription. These are applied directly to the nail, but they only help a very small number of fungal nail problems.
- Oral Terbinafine can be prescribed by your GP if deemed suitable as they can affect kidney and liver function.
-
How to access the service
In hospital, you can be referred to the podiatry service by medical staff for assessment and advice.
In the community, you can contact the service directly through the referral number listed below. You can also ask a GP, family member or other healthcare professional to do it for you.
Central Booking Service: 02871 864399
Referral lines are open:
Monday to Thursday from 9:00AM – 5:00PM
Friday from 9:00AM – 4:30PM -
Useful Links
Health and Care Professions Council
Resources for those with Diabetes:
- Download and Print the ‘Taking Care of Feet’ Leaflet
- Download and Print the ‘Low Risk’ Leaflet
- Download and Print the ‘Moderate Risk’ Leaflet
- Download and Print the ‘High Risk’ Leaflet
- Download and Print the ‘Looking After Diabetic Ulcer’ Leaflet
- Download and Print the ‘Holiday Feet’ Leaflet
- Download and Print the ‘Charcot Foot’ Leaflet
Patient information on:
Information on Common Foot Problems:
-
Further Resources
Taking Care of Your Feet – Patient Resource – Download and Print

Podiatry Department Foot Health Advice Leaflet
Taking Care of Your Feet – Fit Feet
- Wash your feet daily. Not too hot, too long or too soapy.
- Ensure to wipe clean between toes to prevent risk of infection.
- Moisturise feet and heels daily but not between toes.
- Cut nails straight across.
- File nails weekly.
- If your feet are sore check them for blisters, calluses, verrucae, rashes or bruises.
- Do not pick or peel at your feet.
- Apply a clean dressing on any wound or scratch.
- Red, swollen or hot toes or discoloured nails, seek advice from your podiatrist, GP or pharmacist.
- Always wear clean socks everyday.
Spot the Difference
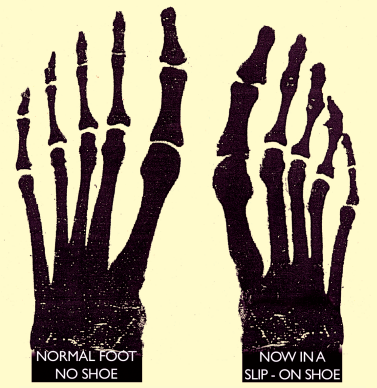
- The space between the toe joints.
- The space between the toes.
- The bones of the feet.
- The length and width of the foot.
FACT! Poor fitting footwear is the main cause of painful callus and corns. Don’t let the size of your shoes bluff you… particularly if you wear slip-ons. Laced shows need to fit your feet differently.
For further information contact your podiatrist.
A podiatrist is an Allied Health Professional (AHP) who deals with diagnosing and managing problems affecting the foot and lower limb. Degree qualified they are regulated by the HCPC to keep the public safe.
For more information contact the Podiatry Dept:
Derry/Londonderry: 028 7186 5100
Omagh: 028 8283 5005 Ext 237437
South West Acute Hospital: 028 6638 2111
Service access is through self and GP referral. It is important that all patients are registered with us for specialist foot health care.
For more information visit:
www.westerntrust.hscni.net/podiatry
www.rcopd.org.uk -
Feedback
We would like to hear more about your experiences. We value all the feedback, whether positive or negative, as this helps us to improve our services.
You can share your feedback through Care Opinion.
Locations where this service is delivered
- Altnagelvin Area Hospital
- Community Services
- Health Centres
- Omagh Hospital and Primary Care Complex
- South West Acute Hospital
- Waterside Hospital
Contacts
Foyle Area
Omagh Hospital and Primary Care Complex
Enniskillen Area




