-
Correct position for bowel motion

- Make sure that your knees are bent and are higher than your hips (it may help to use a footstool/toilet rolls).
- Lean forward from the hips, with your hands or elbows resting on your thighs.
- Bulge your tummy muscles forward as you take a deep breath in and then allow your waist widen . This allows us to relax our pelvic floor.
- Make sure you breath and keep your mouth open, some people talk or make a noise like the ‘moooo’ or pretend to blow through a straw
- Slowly relax, drawing up gently through your back passage to finish.
You may need to use your hand to support / splint upwards on your vulva region to help pass a poo more easily.
-
Post Natal Physiotherapy Management of Scar Tissue
The following explains the management of post natal scar tissue in the perineal area.
Postnatal perineal scar massage
If you have had an episiotomy or a perineal tear, the scar tissue around the area can become tight and may become attached to layers below. This may cause discomfort during intercourse and during activity. By massaging the perineal area, you can reduce your scar tissue.
When should I start massaging?
Wait until you have had your postnatal check which is usually at six weeks. Ensure your stitches have fully healed before beginning. You should not start massage if you have any vaginal infection as this could make it worse.
The perineal area

How to massage the scar tissue?
- It helps to have had a warm bath or use a warm compress before starting in order to help to relax the muscles and increase blood flow to the area.
- Make yourself comfortable: lying or semi sitting, using pillows.
- Use oil or lubrication for comfort – e.g. almond, coconut or olive oil (as long as you are not allergic to it)
- You should massage the scar tissue in three directions for 5-10 minutes a day
Technique – Perineal massage
- Start externally. With your thumb or fingers as below apply pressure and firmly massage into the scar along the line of the scar, across the scar and in circles over the scar. Work over all parts of the external scar towards the anus.

- For internal stitches, get into a comfortable position with your legs gently opened. Insert your thumb into the entrance of your vagina so the pad of your thumb is facing down towards the anus. Place your index finger over your perineum; you should be able to feel the scar beneath your finger.
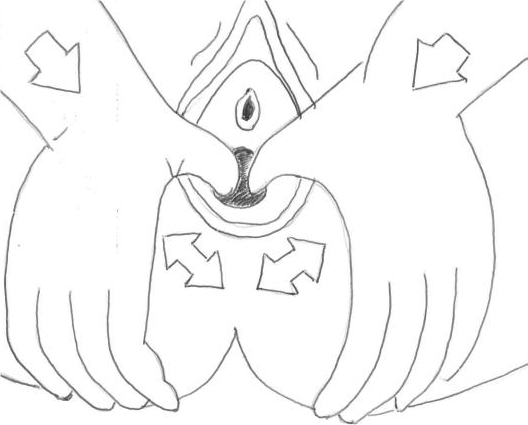
- Next, apply a firm pressure on the back of the vaginal opening with your thumb and make firm “U” shapes (going from 4 to 8 as if imagining a clock) over the scar area. This might feel a little bit tender to start with.
Download Post Natal Physiotherapy Management of Scar Tissue information
Related Resources
-
Constipation - Lifestyle and Diet Education
What is Constipation?
Constipation is defined as having less than three bowel motions per week with stools that are difficult or hard to pass. They may require you to push, strain, digital extract or you can feel incompletely empty.
Untreated constipation can put stress on your bladder and pelvic floor muscles/ fascia, weakening them over time, which may lead to pelvic floor issues later on. Straining to pass a bowel motion can lead to haemorrhoids (the veins in the rectum become swollen and itchy).How to Manage Constipation
Fluids
Pregnant and Breastfeeding women need to increase their fluid intake. Breastfeeding women should increase it to about 3 Litres. Having a glass of warm water in the morning can help to get your bowels moving first thing.
Foods
Try to eat foods that are more ‘watery’ in texture, or hold water in. e.g chia seeds, psyllium husk, soups, stews, pears, kiwi fruits, berries, salads, whole grain bread, brown rice, dried fruits and green vegetables.
Avoid foods that may worsen constipation, such as bananas, white flour, white rice, processed foods, dense heavy breads and too much red meat.
Toileting
- Make sure that your knees are bent and are higher than your hips (it may help to use a footstool/toilet rolls).
- Lean forward from the hips with a straight back.
- Gently bulge your tummy muscles forward as you take a deep breath in and then allow your waist to widen. This allows us to relax our pelvic floor.
- Make sure you breathe and keep your mouth open, some people talk or make a noise like the ‘moooo’ or pretend to blow through a straw, so to fully relax your pelvic floor and prevent straining and contracting your pelvic floor.
- Use hand to splint upwards on the vagina, to help passing a poo
Exercise
Trying to walk continuously for a minimum of 20mins every day can really help to get the bowels moving.
First thing in the morning
After your cup of warm water, try some abdominal massage
Stool softeners
Speak to your GP, Pharmacist, to see if this is something you may need to help your stools to a softer consistency.
Further management
If these strategies do not improve your symptoms, make an appointment with you women’s health physiotherapist, as they may need to assess your pelvic floor by carrying out a vaginal/rectum examination.
Download Constipation; Lifestyle and Diet Education information
-
Diastasis Rectus Abdominus (stomach separation)
Diastasis Rectus Abdominis (DRA) is the thinning and widening of the linea alba, which is a thick band of connective tissue in the midline of the abdominal wall.
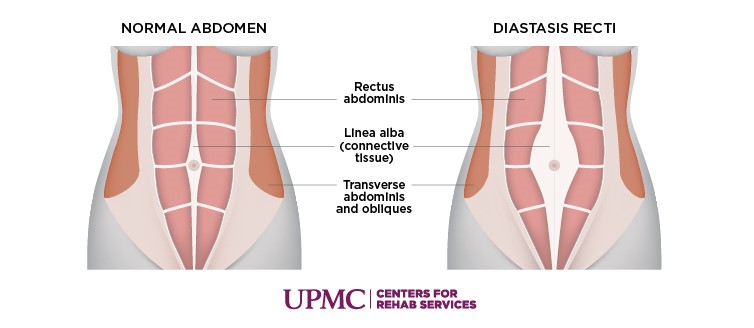
It is a very common and normal change affecting up to 66-100% of women in the 3rd trimester and should be considered a relatively normal change postpartum unless it is significant.
What is significant?
We all have a ‘gap’ to start with. The normal distance between the muscles is around 2cm (around one finger width) in women who have never been pregnant. Researchers found that the gap can be considered NORMAL up to 3 cm postpartum. If your tummy separation is larger than this you should continue to follow this advice on this leaflet. A small bulge may be visible called ‘doming’. Remember it is not all about the gap, as physios we are concerned about the function of the abdominal wall.
How can I help it?
Support garments
There are a range of support garments available for women postnatal, with the idea of bringing the muscles closer together to facilitate healing. However there is no good quality research to support their use, but that is not to say some women find them very beneficial in the early weeks following birth. Your Physiotherapist can guide you on recommendations.
Exercise
Current physiotherapy practice is based on establishing correct activation of the deeper layers of the abdominal muscles and progression of exercises to work the muscles in a functional way. This is best achieved by an individual assessment and prescription of suitable exercises for you. Postnatal exercise classes are a great way to help recovery from the inside out, for example postnatal Pilates.
You can activate the deep layers of the abdominal muscles by doing the following exercise:
Abdominal Activation
You can do this exercise in a comfortable position e.g. lying on your back with legs bent
- Breath in and relax your tummy
- As you breath out, gently draw in your lower stomach muscles, aim to hold for 5 sec and breath
Posture
Improving posture can help abdominal muscles to work more effectively throughout the day. If you need to lift something make sure use the correct lifting technique – Bend knees, tighten pelvic floor muscles, tighten your deep abdominal muscles and breathe out as you lift.
Good bowel habits
Constant straining or pushing on the toilet may affect or worsen a DRA. You should talk to your health care professional for advice.
Top tip would be to use a foot stool to help reduce straining.
Download Diastasis Rectus Abdominus (stomach separation) information
If you have any ongoing issues or concerns about your stomach muscles please contact your GP for a pelvic health physiotherapy referral.
-
Physiotherapy Management of Caesarean scar
It takes approximately six weeks for your scar to heal fully. It may feel tender, itchy and numb in the first few weeks and can heal to be pink or red and slightly raised. Once healed, it should not be excessively painful or sensitive or prevent you from doing any of your everyday activities. It can take two years for your scar to fade to a smooth white line. As your scar heals, the scar tissue can attach to the skin and muscles around it which can make the scar sensitive, painful or raised. Scar massage can help reduce these adhesions. Wait until your scar is fully healed before starting scar massage – there must be no open areas or scabs. Check with your GP or Consultant before you begin if you have concerns.
How to massage caesarean section scar?
- It helps to use a warm compress before starting to help in order to relax the muscles and increase blood flow to the area
- Make yourself comfortable: lying or semi sitting, use pillows.
- You can use oil for comfort e.g. almond, coconut or olive oil.
- Aim to do this for ten minutes per day.
Technique for Caesarean section massage
Start by gently massaging around the scar, focusing on tissues immediately above and below it. As it becomes less sensitive, place the pads of your fingertips just above the scar line. Move the skin gently up and down, side to side and in circles along the length of the scar. Work more into areas of resistance where the skin feels tighter. You should feel stretching in the tissue but it should not be painful.
As this becomes easier, push your fingers firmly down into the tummy muscles and repeat the up and down, side to side and circular movements. Feel free to massage the entire lower tummy area. You must be firm but not aggressive as you massage: let pain be your guide. A slight tingling sensation as you stretch tissues is normal. Keep massaging into deeper areas as pain allows.
When you are comfortable with the first two, roll the scar between your thumb and finger. It may take some days or weeks before you can do this one below.
Continuing problems and when to seek advice
If you have any of the problems below seek advice from your GP, who can then refer you to a Women’s Health Physiotherapist:
- Excessive weakness around the abdominal area
- Heaviness/bulging sensation in your perineal area
- Any problems with loss of bladder or bowel control – such as wetting, soiling or having to rush to the toilet.
- Difficulties or pain with sexual intercourse
Download Physiotherapy Management of Caesarean Scar information
Related Resources
-
Bladder Diary
This resource can be used to record and track bladder urge, leaking, urine volume and fluid intake.
-
Perineal massage
What is perineal Massage
Perineal massage is a method of preparing the outlet of the vagina for the stretching and pressure sensations during the birth of you baby.
When you should avoid perineal massage
- Prior 34 weeks of pregnancy
- If you have any vaginal herpes, thrush or any other vaginal infection
- Severe blood pressure problems in pregnancy
- Concerns regarding the growth of your baby
- If you have any cervical shortening (also known as incompetent cervix)
- Placenta praevia (low lying placenta) or any other conditions where there is bleeding from the vagina
Benefits of perineal massage
- Perineal massage helps your ‘mind-body’ connection, helping you to be more aware of the area for when in labour
- It may help to lower the risk of tearing (vagina to anus) that required stitches or episiotomy (surgical cut to the perineum) for first time moms.
- Women tend not to report the extremes of stinging and burning that often accompany the birth of their baby’s head
- Perineal massage can decrease the chance of ongoing perineum pain at three months post-delivery.
How to perform perineal massage
- 2-3 times a week from 35 weeks of pregnancy
- Bath or warm compresses on the perineum prior perineal massage can help to relax the area.
- Empty your bladder if you need to pass urine, wash your hands and find a relaxing comfortable position (in the bath relaxing legs to either side of the bath, bed, legs supports with pillows)
- Using a mirror can help you become familiar with the vaginal opening
- You or your partner can carry out the perineal massage. * your partner will need to have clean hands and gently insert one index finger into the lower part of the vagina, you must tell your partner how much pressure to apply.
Technique
- Apply, a water-soluble lubricant or natural oil (olive oil) on one or both of your thumb
- Place one thumb just inside the vagina entrance, working from nice down to six and up to three, thinking of a clock face. Avoid pressing on the top part of the vagina.

- Gently press down, hold and relax with the pressure, slowly move from 9 to 3 to gently stretch the vagina opening

- You can experience a strong stretching burning sensation the first few times, this should ease over time
- Perineal massage can be done for up to 10 mins, daily
-
Pelvic Floor Muscle 3D Animation




